Neat Little Guide — 26 minutes
Sleep disorders
Getting a good night’s sleep is critical to our overall health and well being, but too many Canadians are falling behind in both the quality and duration of sleep. If you’re not getting the sleep you need it’s important to understand the reasons why, and to understand how to make the practice of good sleep hygiene a part of your life’s routine.
Sleep: Your Health’s Best Friend

Sleeping is one of the human body’s most critical biological functions — just as important as breathing, eating and digestion, and the beating of our heart. About a third of our life span will be spent sleeping, an absolutely necessary period of restoration for which there is no substitute. Even a minimal disruption in our sleep cycles can have a significant impact on our health and wellbeing, in both the short and long term.
We may think that our bodies are inactive and our minds are resting as we sleep, but in reality there’s a lot of essential electrical activity going on in our brain and other core functions. While sleeping, the body is hard at work recharging for the next day, fighting off infections, replenishing our capacity for memory and learning new skills, reducing stress and improving overall mood. All that, and much, much more.
Unfortunately, many of us don’t sufficiently value the quality or duration of our sleep. We allow obligations and commitments to cut into our sleep time. Instead of going to bed at a reasonable hour, we are doing other things — office work, bookkeeping, watching television, or scrolling on our phones — that may seem more important than going to sleep. If you are having trouble sleeping, you are not alone. According to Statistics Canada [1]
- 43% of men and 55% of women aged 18 to 64 report experiencing sleep problems "sometimes, most of the time or all the time [2].
- 33% of Canadians sleep less than 7 hours a day (the recommended amount of sleep for 18-64 years old is about 8 hours) [2].
- Parents with two or more children sleep 25 minutes less than Canadians without children, while parents with only one child sleep 17 minutes less.
A “good night’s sleep” means something different for everybody, but the habits that get you there are consistent. Practising good sleep hygiene is so important to our overall health, and the adverse effects of not regularly getting a good night’s sleep are manifold. What happens to your metabolism at night is just one example – when we don’t sleep well we don’t metabolize properly, and that can negatively affect our diet by causing us to eat too much or eat unhealthily during the day. If you’re diabetic, having a bad sleep can make it especially hard for to control your symptoms.
The intention of this guide is to provide you with the knowledge and tools to help improve your sleep hygiene, ensuring your mind and body benefit from more restful nights, and hopefully enhancing your overall quality of life.
Find answers with our online sleep assessment form.
The Science of Sleep
Frequent waking or sleepless nights can be extremely detrimental to your health. The quality of your sleep is important in order to feel refreshed and rested when you wake up. After a good night’s sleep, your energy levels are usually higher the next day. Deep sleep allows your body to recover and helps restore your muscles and tissues while strengthening your immune system. During REM sleep, your mind recharges, which explains the vital role of good sleep in learning and memory.
If you slept well, you feel rested when you wake up. You did not sleep well if:
- The sound of your alarm clock makes you want to go back to sleep
- Getting out of bed is hard
- You feel as tired as when you went to bed the night before
- You yawn all day, and minutes seem like hours
- You are irritable, hypersensitive or impatient
The Impact on Your Health and Well-being
Sleep disorders, in all their forms, can have serious effects on your physical and mental health.
Consequences of Inadequate or Disturbed Sleep (short term)
- Problems with concentration and memory
- Decreased vigilance
- Fatigue
- Irritability
- Emotional fragility
- Increased appetite (weight gain due to disruption of leptin and ghrelin hormones that help control appetite)
- Risk of motor vehicle accidents
Consequences of Inadequate or Disturbed Sleep (long term)
- Impact at school or work, social life as well
- Decreased immune system
- Risk of obesity
- Risk of diabetes
- Risk of cardiovascular disease
- Risk of certain cancers
- Risk of depression
- Risk of high blood pressure
Sleep Cycles and Structure
“Sleep” is not a single, constant state – what your body is up to during sleep will vary over the course of a night. The various stages follow one another to constitute a series of 90- to 120-minute sleep cycles. During your sleep, each cycle, composed of 4 distinct stages, repeats itself 4 to 6 times. So if you go to bed at 10:30 pm, the first cycle ends at midnight with the others following throughout the night.
Stage 1
- Falling asleep, sometimes accompanied by muscle contractions or jerking motions
- You are between wakefulness and sleep. This period is generally short.
- You are aware of any surrounding noise
Stage 2
- Slow-wave light sleep — eye movements stop, heart rate slows, body decreases in temperature.
- You spend between 45 and 55 percent of your night in stage 2. This stage is important for your physical and mental health, among other things.
Stage 3
- Slow-wave deep sleep — brain waves slow down but heighten in amplitude.
- This stage is important for physical recovery, strengthening of the immune system, appetite control and growth, among other things.
Paradoxical Sleep Stage (or REM, for “Rapid Eye Movement”)
- You start to dream
- Your heart rate and breathing accelerates and your blood pressure increases
- Your eye movements become rapid and irregular
- The muscles in your arms and legs are paralyzed
During the night’s earlier cycles, you spend more time in stage 3. The longer the night progresses, the longer the REM stages. If you have been deprived of sleep, your body first tries to catch up on its deep sleep (stage 3) and REM sleep.
No one stage of the sleep is more important than any other. It is the continuity of the cycles that is important.
An adult needs about 8 hours of sleep per night, but for some people, 6 hours is enough and for others, 10 hours is required. You will know what feels right for you.

Types of Sleep Disorders
There are several types of sleep disorder that cause cognitive or behavioural issues. If you think you may be suffering from a sleep disorder, your doctor can refer you to a specialist for diagnosis and a recommended treatment.
Disorders as defined in the International Classification of Sleep Disorders (ICSD):
Insomnia (acute or chronic)
Insomnia is characterized by difficulty falling asleep or staying asleep, resulting in the person being dissatisfied with the duration and quality of their sleep.
There are three types of insomnia:
- Onset insomnia: Difficulty falling asleep at night
- Maintenance insomnia: Waking up in the middle of the night and having trouble falling asleep again
- Terminal insomnia: Waking up too early in the morning
In addition to experiencing sleep difficulties at least three times a week, a person suffering from insomnia may have the following symptoms during the day: irritability, excessive fatigue (physical and mental), as well as difficulty concentrating.
Insomnia can be caused by poor sleep hygiene, physical factors such as pain or illness, or psychological factors such as depression.
Insomnia is one of the most common sleep disorders. An estimated 25% of Canadians have experienced symptoms of insomnia lasting for more than a year. It can affect anyone, even children, but is more common among women, the economically disadvantaged and those in poor health.
Hypersomnia and narcolepsy
Idiopathic hypersomnia
Hypersomnia, also known as hypersomnolence, is characterized by excessive sleepiness or uncontrollable bouts of drowsiness during the day. When these symptoms are due to a lack of sleep, a disorder such as obstructive sleep apnea, an illness, overwork or the use of certain medications, the condition is known as secondary hypersomnia.
When symptoms are not related to any particular disease or behaviour, we use the term primary hypersomnia. There are three types of primary hypersomnia: narcolepsy (see below), Kleine-Levin syndrome, a very rare neurological disease associated with cognitive and behavioural problems, as well as idiopathic hypersomnia.
This condition may take the form of chronic daytime drowsiness or extended periods of sleep (more than 10 hours per day). It may include difficulty waking up and getting out of bed, as well as confusion upon awakening, trouble staying awake during the day, extreme fatigue or attention deficit.
The causes of idiopathic hypersomnia are not well known, but this neurological disease could be due to a malfunction of the arousal systems. This rare disease affects 0.01 to 0.04% of the population, men and women alike.
Narcolepsy
People who suffer from narcolepsy are prone to falling asleep abruptly at any time. They could be talking to someone, driving a car or doing housework. Brief episodes of cataplexy, which is a loss of muscle tone in part of the body, can also occur in response to intense emotions such as surprise, laughter or anger, and can cause the person to fall.
In some cases, upon awakening or just before sleep, narcoleptics experience a brief paralysis that may be accompanied by hallucinations, making this disorder especially frightening. As if that were not enough, the quality of their sleep is also poor.
This rare disease, which affects about 0.05% of the population, varies considerably in intensity. It can cause multiple sleep attacks per day, lasting from a few minutes to nearly an hour, or only a few episodes per year.
The causes are not well known. Hypocretin (also known as “orexin”), a neurotransmitter responsible for waking up, has been found to be lacking in the brains of people with this disorder. Some studies suggest that an autoimmune reaction completely destroys the nerve cells that produce hypocretin.
Circadian rhythm disorder
Also known as sleep-wake disorder, circadian rhythm disorder involves a disruption of the biological clock where sleep is not synchronized with the day and night cycle. People who suffer from this disorder may have trouble falling asleep or staying asleep, feel drowsy during the day or be unable to function as well as usual.
There are several types of circadian rhythm disorder:
Delayed sleep phase. Falling asleep and waking up more than two hours after the normal cycle. The person may have a normal amount and quality of sleep, but has difficulty falling asleep and waking up at times that are considered acceptable or beneficial. This disorder is more common in adolescents and young adults.
Advanced sleep phase. Falling asleep and waking up much earlier (at least two hours, often more) than usual. The person may have a normal amount and quality of sleep, but will feel drowsy in the late afternoon and wide awake in the early morning. This disorder is more common in the elderly.
Irregular sleep-wake rhythm. Sleep is fragmented into short periods throughout the day and night. In total, the person may get a normal amount of sleep, but the fragmented nature of the sleep can be disruptive and affect their social life. This disorder is more prevalent in the elderly.
Free-running syndrome. Falling asleep and waking up are increasingly out of sync with the normal schedule, because the sleep-wake cycle is not tied to the 24-hour cycle, but to a slightly longer period. This means that the person falls asleep and wakes up a little later each day. This disorder is quite common among the blind population, as daylight usually helps regulate the sleep-wake cycle.
Shift work sleep disorder. This disorder mainly affects people who work night shifts. Because their work schedule does not match their circadian rhythm, they may experience an irresistible urge to sleep on the job and an inability to sleep when they need to. When they do sleep, the quality is often poor, leading to fatigue, exhaustion, headaches, difficulty concentrating and irritability. Some studies suggest that 5-10% of shift workers suffer from this disorder, while others estimate the prevalence to be as high as 30%.
Jet lag. This disorder occurs when a person crosses multiple time zones. Because the body’s internal clock is still based on the original time zone, the person may experience a strong desire to sleep during the day and an unwanted level of alertness at bedtime. Jet lag is temporary; it is estimated that the body needs one day to adjust to each time zone crossed.
Parasomnias
Night terrors
Night terrors are episodes of intense confusion and fear that occur for no apparent reason during slow-wave sleep, usually between one and three hours after falling asleep. Unlike a nightmare, the person is not aware of what they are doing and does not remember the episode when they wake up.
The manifestations are very disconcerting. The person may bolt upright in bed, start screaming or sobbing, struggle or talk incomprehensibly. These symptoms may be accompanied by sweating, shortness of breath and a rapid heart rate.
An episode lasts from one to five minutes, sometimes up to 20 minutes, and then the person falls back asleep with no difficulty. Since they have no memory of the episode, it is best not to awaken or interact with them, or talk about it when they wake up.
Night terrors can be caused by fatigue, a high fever or a stressful event. They may also be due to a genetic predisposition.
Night terrors are more common in children, especially those aged three to six, and tend to disappear spontaneously before adolescence.
Sleepwalking
Sleepwalking happens when a person exhibits motor activity during the early stages of slow-wave sleep, usually one to three hours after falling asleep.
The sleepwalker may simply sit up in bed, or get up and walk around. They can do simple things like opening a door, descending stairs or performing everyday tasks. This condition is benign, but it can put the person at risk of injury.
These occasional behaviours rarely last more than about 10 minutes. The person may then wake up on their own or return to bed. They will have no memory of what happened. Since it may be difficult (but not dangerous) to wake them up, it is best to gently guide them back to bed.
A number of causes can lead to sleepwalking, such as stress, puberty, fever or a lack of sleep. It may also be due to a hereditary factor.
Sleepwalking is more common in young children than in adults and tends to disappear with time. About 15% of children between the ages of 5 and 12 will experience at least one episode of sleepwalking.
REM sleep behaviour disorder
REM sleep behaviour disorder is characterized by the occurrence of motor behaviours during REM sleep, in contrast to sleepwalking, which occurs earlier, during the slow-wave sleep phase.
Usually, the body is unable to move during REM sleep. A person with this disorder does not experience this muscle atony and may exhibit behaviours, often violent, that usually reflect what they are dreaming about. They may start talking, shouting, gesticulating and even kicking. When they are awakened they may remember, for example, that they were trying to save someone in danger.
REM sleep behaviour disorder can be due to the use of antidepressants, alcohol withdrawal or sedative medications. It can also be associated with neurodegenerative illnesses such as Parkinson’s disease, or have no specific cause. Affecting around 0.5% of the population, it most often appears after the age of 50, especially in men (87% of cases).
Abnormal movements related to sleep
Restless Leg Syndrome (RLS)
Restless legs syndrome (RLS) is a feeling of discomfort in the legs and sometimes the arms when the person is sitting or lying down. Symptoms include itching, electric shock, pain, tingling, pins and needles, etc. The person feels an uncontrollable urge to move their legs, which can make it difficult to fall asleep. This urge increases in the evening and at night, and the movements may even occur involuntarily during sleep (see “Periodic limb movement disorder” below). In the long term, these constant movements lead to fatigue and drowsiness during the day.
There are two types of RLS. The first type seems to have no known cause and is thought to be related to heredity. The second is believed to be associated with a lack of dopamine in the brain, caused by iron deficiency or a chronic illness such as diabetes, kidney failure and hyperactivity. Pregnancy can also cause or worsen symptoms.
RLS is estimated to affect about 10% of the Canadian population. It can occur at any age, especially after age 50, and particularly in women, who are affected twice as often as men.
Periodic limb movement disorder
In people who suffer from periodic limb movement disorder (PLMD), the legs and sometimes the arms twitch repeatedly during the night, causing micro-awakenings that can disrupt sleep and lead to daytime drowsiness. People with this disorder are not aware of their movements, but they may disturb their partners, who feel as if they are being kicked.
This disorder is common in people with RLS, but it can also occur alone or with other sleep disorders, such as sleep apnea and insomnia. It is estimated to affect 10-15% of the population.
Bruxism
Commonly known as teeth grinding, bruxism involves clenching the lower and upper teeth tightly and moving them back and forth, causing pain in the jaws and gums, as well as wearing down of the teeth, headaches and even damage to the temporomandibular joint. This grinding is involuntary and can happen, with no conscious effort, while the person is awake or sleeping.
Bruxism during sleep is the most common type and the hardest to control. It is thought to be caused by stress and anxiety, but can also occur in people suffering from illnesses such as sleep apnea or Parkinson’s disease, or with a family history of bruxism. Smoking, caffeine and the use of certain antidepressants or recreational drugs can also increase the risk.
Bruxism is more common in young children, but is believed to decrease with age. It is estimated that about 15% of children and 8% of adults grind their teeth a few times a week.
Sleep disorders linked or related to breathing
Sleep Apnea
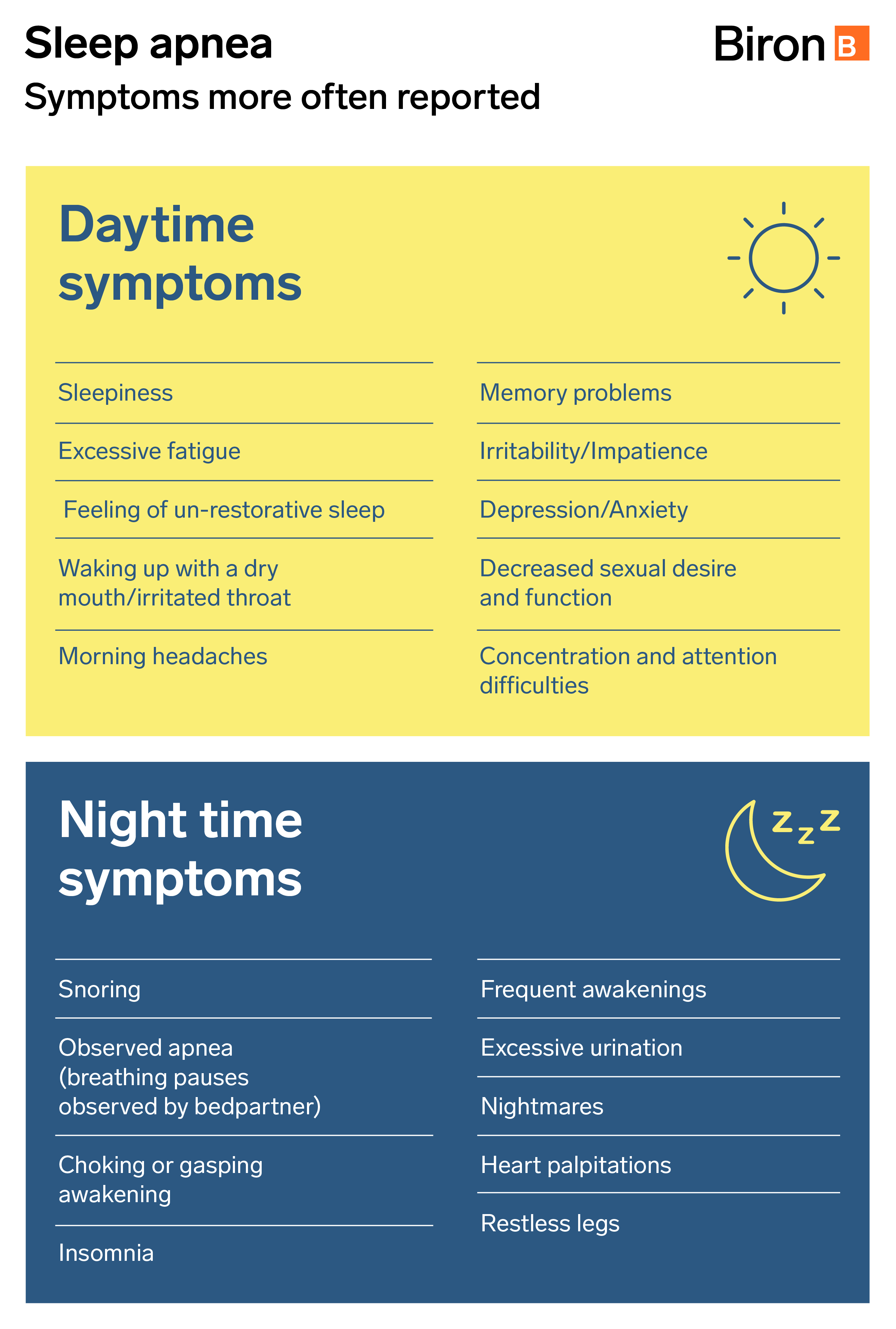
Sleep apnea is a breathing disorder associated with sleep. Respiratory obstruction of the pharynx (at the throat level) may be complete (apnea) or partial (hypopnea) and it can cause a decrease in the blood oxygen level (hypoxemia), an increased heart rate and/or microarousals. These microwakes are very short, they can occur regularly during the night, and though you won’t be aware of them, they will disrupt your normal sleep cycles.
On average, these breaks last 10 to 30 seconds, until the brain responds to the problem. Each time, your sleep is disturbed, even if you don’t fully wake up and have no memory of waking up. These respiratory stops are repeated throughout the night, disrupting the sleep pattern you need to complete to feel rested and awake in the morning.
There are two types of sleep apnea. The most common type is the obstructive sleep apnea that occurs when your upper airway is obstructed during your sleep. Central sleep apnea occurs when, for a variety of reasons, your brain does not report to your body that it must continue to breathe. Mixed sleep apnea occurs when a person suffers from both types of apnea, obstructive and central.
Two Types of Sleep Apnea
You may be aware that obesity is one of the primary causes of obstructive sleep apnea, but it’s important to know that it’s not the only one. Though the risk to obese people is four times higher, 40 percent of people with obstructive sleep apnea are not obese. You can be a tall and thin person and have this sleep disorder. Other risk factors include:
- A family history of sleep apnea
- Narrowed airways
- Neck circumference (excess weight around neck can narrow airway when laying down)
- Small jaw: recessed chin
- Tonsils become enlarged
- Age
- Consumption of alcohol, tobacco, sedatives and tranquilizers
- Nasal congestion
In this case, breathing is not obstructed, but rather the respiratory system is not getting the biofeedback signal it requires to breath. Risk factors include:
- Age
- A history of heart problems
- Drug use
- Stroke victims
Tips for Better Sleep Hygiene
Good sleep hygiene can help prevent certain sleep disorders or reduce their consequences. It can also help in cases of sleep apnea, though it will not actually treat the condition or make it go away; for that you need proper treatment.
It is important to relax before bedtime and, as best as possible, always go to bed at the same time. A routine before bedtime helps the body and brain to slow down, reduces the stress of the day and promotes falling asleep.
Here are a few tips for practicing better sleep hygiene:
- Avoid stimulants such as alcohol, caffeine and nicotine, or intense exercise near bedtime
- As your bedtime approaches, relax (read, listen to music, take a bath) and stop all interaction with your electronic devices (smartphones, Internet, TV)
- Learn to recognize when you are getting sleepy (e.g. nighttime chill, heavy eyelids). If you’re working night shifts, watch for the sensation of sand in the eyes
- Keep your bedroom environment calm, dark, and comfortable
- If you’re still awake after 30 minutes, get up and do a monotonous or repetitive activity that doesn’t require physical effort but does require mental effort (reading, crossword puzzle, sudoku). These activities will tire your brain without physical stimulation. As soon as you feel the signs of sleep, go back to bed
- Go to sleep and wake up at the same time every day
Diagnosis and Treatment
A sleep study is essential to make an accurate diagnosis of sleep apnea. During a consultation, your doctor will give you a prescription for an examination. Polysomnography is a test that you undergo in a laboratory for an entire night, while cardiorespiratory polygraphy is a simplified test performed at home.
Although there are several treatments available for sleep apnea, the preferred treatment for all types of apnea remains the continuous positive airway pressure (CPAP) device. However, depending on the severity of your sleep apnea, your doctor may suggest other treatment options, including the following:
- Changing certain lifestyle habits, such as losing weight, having better sleep hygiene, limiting alcohol consumption, quitting smoking, etc.
- Wearing a mandibular advancement device
- Undertaking positional therapy
- Undergoing surgery
We can diagnose sleep apnea and other sleep disorders and assess the best treatment options for you. Our team of trained sleep care professionals are here to listen to your needs, and will be there for you before, during, and after examinations to provide you with personalized and tailored treatment options that make sense for your lifestyle.
At Biron, we offer a range of services covering all aspects of diagnostic testing. Learn more!
Sources2
- Statistics Canada. Duration and quality of sleep among Canadians aged 18 to 79. https://www150.statcan.gc.ca/n1/pub/82-003-x/2017009/article/54857-eng.htm
- Statistics Canada. Sleep behaviours among Canadian adults: Findings from the 2020 Canadian Community Health Survey healthy living rapid response module. https://www150.statcan.gc.ca/n1/pub/82-003-x/2022003/article/00001-eng.htm







