Blood tests and blood samples
Have you been prescribed laboratory blood tests by your doctor?
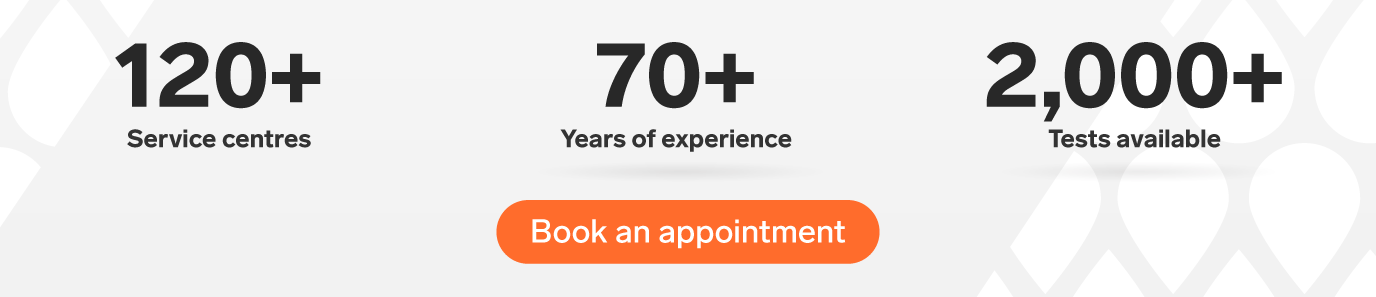
Biron Medical Laboratory offers blood test services and other sampling, including urine samples, and throat and stool samples. Choose the best location for you to have your sample taken: at a private clinic, at home or at work.
ISO-accredited laboratory

Certified, experienced, courteous staff

Fast results

Costs covered by most private insurers

Did you know? A medical prescription is required
In Quebec, a blood test has to be prescribed by an authorized healthcare professional, like a doctor or a nurse.
What happens during a blood test?
Booking an appointment
To book an appointment:
- Book an appointment online or calls us at 1 833 590-2712
- Go to one of our private walk-in clinics
- Schedule an appointment online or by phone to have the sample taken at home

Preparing for the blood test
Fasting or any other special preparation are rarely needed.

Sampling
It only takes about 15 minutes for nursing staff to check the prescription and assess your needs, before taking the sample.

Rapid results and support
Your results are sent to you and your treating doctor quickly, with complete confidentiality.

We offer a wide range of testing, including thyroid and biochemical, complete blood counts, blood sugar testing and screening tests.
How much does it cost for a blood test or sampling at Biron?
Costs depend on the number and type of tests on your medical prescription. For example, the cost of a standard blood test is between $150 and $250. This cost typically includes 15 minutes of service by a certified nursing staff member and the costs of the laboratory tests. The expenses may be reimbursed by private or group insurers. We recommend checking with your insurer before doing any tests.
Get an estimate of the costs for tests by starting the process of booking an appointment online or by calling 1 833 590-2712.
Frequently asked questions
Is my prescription valid?
In Quebec, blood samples must be prescribed by an authorized healthcare professional such as a doctor, dentist, pharmacist, midwife or nurse, based on their field of practice. Prescriptions issued by naturopaths, osteopaths, homeopaths, chiropractors and acupuncturists are not accepted.
Who can take my blood sample?
In Quebec, blood tests are exclusively done by doctors, nurses or medical technologists. Respiratory therapists and radiology technologists may also take some blood samples while practising their specialty.
How can I prepare myself for my blood test?
Fasting is rarely necessary for interpreting results properly.
When you book an appointment, if necessary, we will provide clear preparation instructions based on the tests to be done, in addition to your treating doctor’s instructions.
How can I find a sampling clinic near me?
There are Biron clinics in many Quebec cities, including Laval, Montreal, Saint-Jérôme, Terrebonne, Saint-Eustache and Repentigny.
What will happen when I go to the service centre for my blood test?
After you show official photo ID, you can get comfortable in a chair with an armrest.
Usually, the blood test will use a vein in your arm. The nurse will wash their hands and briefly put a tourniquet (band made of rubber) around your arm to make the veins more visible. You may be asked to temporarily clench your fists to make your veins stand out more. They will wash and disinfect the skin before inserting the needle, fitted with a cylinder, in the vein. The cylinder makes it possible to fill all the collection tubes needed without having to change needles.
In some cases, when the veins in the arm are difficult to use, a “micro-method” blood sample may be taken by pricking the end of the finger. This approach uses smaller collection tubes and is often preferred for very young children.
Once all the samples have been taken, the needle is removed, and light pressure is applied to the puncture site until the bleeding stops. A small adhesive bandage may be applied. Each collection tube will then be labelled with your name and any other relevant information. It is important to check that every tube is identified with your name.
What are the potential side effects of a blood test?
Usually, there are no side effects with a blood test. Some people may feel a little prick or a burning sensation when the needle is inserted in a vein in the forearm. It is also possible to feel a little discomfort when the needle is removed.
In rare cases, especially with complex sampling (hard-to-find veins or a needle that moves), there may be slight swelling or bruising at the sample site. Those reactions usually go away in a few days.
How will I get the results?
Your results will be sent electronically, either through MyBiron or by email, in a password-protected PDF file. They will also be sent directly to the healthcare professional who issued your prescription.
How much blood is taken?
The amount of blood taken is very small. A lavender stopper tube for a complete blood count holds 4 mL of blood, less than a teaspoon, while the larger tubes, for biochemical and other testing, will hold about a teaspoon and a half of blood. More elaborate blood testing, requiring four or five collection tubes, only requires just over a tablespoon (15 mL) of blood, a tiny fraction of the four to five litres of blood in our bodies.
How are specimens stabilized and stored?
Once the blood has been drawn, the collection tubes are stabilized before transport to the laboratory. Tubes containing anticoagulated blood are usually refrigerated until they are tested in the lab. Serum tubes need to be centrifuged quickly to separate out the serum before they are refrigerated.
Biron uses the best specimen stabilization practices. The temperature of containers used to transport tubes from the sampling centre to the lab is monitored to prevent any exposure to unsuitable temperatures (too hot or too cold).
How does Biron support patients while providing service?
At Biron Medical Laboratory, we offer patients personalized, instant support. Certified nursing staff take time to welcome patients into a private room, where they check the prescription, make sure that all the prescriber’s pre-test requirements have been met and assess anxiety levels before collecting the sample.
Our sampling centres are clean, quiet, friendly and modern. Biron Medical Laboratory also makes results available to patients through an online platform, allowing patients to take charge of their own health. Biron laboratory experts are available to discuss the interpretation of your tests with you or your doctor. Your personal information is kept confidential throughout the entire process.
How does Biron Medical Laboratory stand out from other labs for blood tests?
Biron Medical Laboratory stands out by using cutting-edge equipment, modern facilities and its accreditations, ensuring the highest compliance levels. The result of these elements is rigorous testing with unprecedented accuracy.
Most mistakes made in laboratories occur in the pre-testing phase and are often due to the wrong choice of test or poor specimen storage. At Biron, our healthcare professionals make sure that all stabilization conditions for specimens are well respected, before and during transport to our central lab.
Any more questions?
Access all our frequently asked questions to learn more about our laboratory, sampling and care services offered.
Learn more through our content
Find the most convenient option for your blood test. Click to learn more!