Specialist Advice — 7 minutes
Shining light on skin cancer: the facts on melanoma
March 4, 2025
Our skin is your body’s largest organ and one of the most important organ [1]. In particular, it prevents the loss of water and electrolytes such as sodium, regulates our body temperature, protects us against infections and produces vitamin D [2]. It contains many different types of cells, including keratinocytes, basal cells, and melanocytes. Each of these cells can eventually show abnormal growth leading to skin cancer.
Is the sun the only cause of skin cancer?
Skin cancer is most frequently associated with sun exposure to the face, the back, the scalp or the lips, but it can also appear in non-sun exposed areas such as the palms, the soles, beneath the fingernails or toenails and genitals. This indicates that there may be other contributing risk factors, such as exposure to toxic substances, or a weakened immune system [3].
Skin cancer is the most commonly diagnosed cancer worldwide. We’re most familiar with melanoma, the type of cancer affecting melanocytes, cells located mainly in the epidermis of the skin. Although non-melanoma cancers (squamous cell carcinoma and basal cell carcinoma) are by far the most frequent types of skin cancer, they generally show slow growth, rarely spread, and are easily treatable. Melanoma represents less than 5 % of all skin cancers but is responsible for more than 75% of deaths from cutaneous cancer [4].
Read also: Myths about cancer mutations
Where does melanoma come from?
Melanoma starts in melanocytes, cells that produce the pigment (melanin) responsible for the colour of our skin, hair and eyes. Melanin is a protective agent against more deleterious sun effects. When melanocytes located in the basal layer of the epidermis are exposed to UV radiation they release melanin, which is taken up by keratinocytes of the upper layers of the skin. This process is responsible for the tanning effect. Too much of this radiation, however, can lead to cell mutation in melanocytes cells and cause melanoma skin cancer.
It is therefore not surprising that non-caucasian individuals with darker skin, since their skin-cells produce more melanin, show a much lower incidence of skin cancer. Conversely, individuals with very pale skin, freckles, light eyes and red hair [6]. At last, caucasian individuals with paler skin living in regions closer to the equator show the greatest risk of developing skin cancer [7].
What are the stages of melanoma?
There are four stages of melanoma development:
- Stage 1 : the disease is localized to a specific area of the skin. Fortunately, the majority of diagnoses are done at this early stage when the condition is more treatable;
- Stage 2 : the disease is more developed, but still localized;
- Stage 3: the cancer spreads to the lymph nodes;
- Stage 4: it moves towards the distant organs.
As with any cancer, the earlier it is diagnosed, the better the chances of curing or at least controlling the disease.
I have a weird mole. When should I consult my physician?
A melanoma often starts as a mole anywhere on the skin. Most people have a few moles, but although not entirely specific, the first sign of a possible melanoma is a change in the colour, size or shape of an already present or new mole.
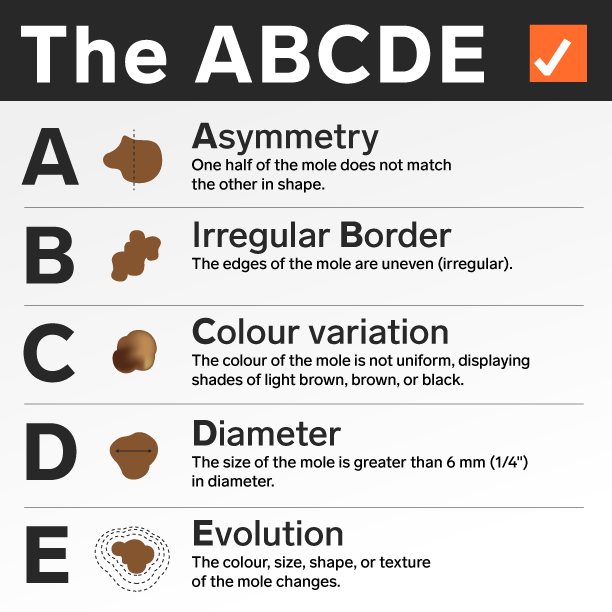
Cancer Canada suggests the ABCDE rule to help you look for other common signs of melanoma skin cancer.
Do not hesitate to consult your doctor if any of these changes appear on your skin. More specific information can be found on the Canadian Cancer Society website. There are also now some apps available for your smartphone that may help you identify problematic moles with your camera.
Treatment of melanoma
Treatment options depend on many factors including the size, type, depth and location of the mole or lesion and your personal preference. Small skin cancers may not require treatment beyond an initial skin biopsy which removes the entire growth. Surgery option, including local excision, sentinel lymph node biopsy, complete lymph node dissection, or surgery for metastases remain the treatment of choice for most melanoma skin cancers. As with many other cancers, immunotherapy, radiation or chemotherapy and targeted therapy with biologicals are the main ancillary treatments after surgery.
Skin biopsy
Microscopic analysis of a skin biopsy taken at the doctor’s office can help identify which type of skin cell (keratinocyte, basal cell, melanocyte, etc.) is growing abnormally and may lead to cancer.
Prevention, prevention, prevention!
Skin cancer is caused almost entirely by sun exposure. It should be evident that protecting our skin from sun exposure is the most efficient (and most economical!) means of preventing melanoma skin cancers. According to Canada Public Health Services, the following recommendations should keep you protected when the UV index is at 3 or higher, indicating a significant risk.
Read also: Sunscreen: dangerous for your health?
Protect your skin
- Cover up: wear light-coloured, long-sleeved shirts and pants, a hat made from breathable fabric, and sunglasses with UVA and UVB protection;
- Limit your time in the sun: stay out of the heat between 11 and 3;
- Use a sunscreen labelled “broad spectrum” with an SPF of at least 30 and preferably water resistant;
- Avoid using tanning equipment. There is no such thing as a healthy tan, and any tanning equipment will damage your skin in the same way that the sun will;
- Ask your doctor, nurse or pharmacist if any of the medications you are taking could be harmful to you when exposed to UV rays.
For professional support, we’re here.
Do you have a skin biopsy scheduled with a health professional? Your sample could be analyzed at Biron for quick results. Talk to your medical team.
This revised edition reflects an updated version from the original version published on our website. We have incorporated recent facts to offer you current and pertinent information.
Sources7
- Goldsmith, L. A. « My Organ Is Bigger than Your Organ. » Archives of Dermatology, mars 1990, vol. 126, no 3, 1990, p. 301-302.
- Société canadienne du cancer. La peau. https://cancer.ca/fr/cancer-information/cancer-types/melanoma-skin/what-is-melanoma/the-skin. Consulted March 4, 2025.
- Mayo Clinic. « Skin Cancer », Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/skin-cancer/symptoms-causes/syc-20377605 , Consulted March 24, 2025. July 2019.
- Santé Canada. Skin cancer. https://www.canada.ca/en/public-health/services/sun-safety/skin-cancer.html. Consulted March 24, 2025.
- Santé Canda. Non Melanoma Skin Cancer. https://www.canada.ca/en/public-health/services/chronic-diseases/cancer/non-melanoma-skin-cancer.html. Consulted March 4, 2025.
- J.X. Wang, M. Fukugana-Kalabis, M. Herlyn. “Crosstalk in skin: melanocytes, leratinocytes, stem cells, and melanoma”. J Cell Commun Signal. August 2006, Vol 10, no3, p. 191-196.
- M. Arnold, D. Singh, M. Laversanne, et coll. « Global Burden of Cutaneous Melanoma in 2020 and Projections to 2040”. JAMA Dermatol. May 2022, Vol. 158, no. 5, p.495-503.
