Specialist Advice — 16 minutes
The low FODMAP diet: A solution for IBS?
Irritable bowel syndrome (IBS) is a common disorder of the digestive system which manifests itself as stomach pain, bloating, flatulence and changes in bowel movements (e.g., diarrhea or constipation). The causes of IBS are not well defined, but some dietary prescriptions play a major role in treating the symptoms. An example is the low FODMAP diet, which eliminates carbohydrates that ferment in the intestinal tract and produce bloating and gas.

What is FODMAP?
The term “FODMAP” stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. These are a series of carbohydrates that are sometimes poorly absorbed by the small intestine and end up in the colon, where they ferment and cause gas. In doing so, they contribute to the symptoms of irritable bowel syndrome.[1]
What are these substances?
Carbohydrates are the body’s main source of energy. They are composed of carbon, oxygen and hydrogen, and are water-soluble, with the exception of fibre. They differ in size and complexity.
Interviewed on the subject, Kathryn Adel, M.Sc, Dt.P, CSSD, Registered Dietitian at SOSCuisine.com and a specialist in sports and gastrointestinal nutrition, made a list of the main FODMAPs:
- Fructose: Found in many fruits, honey, agave syrup, molasses or high-fructose corn syrup (added to sweeten various processed foods)
- Lactose: Found in dairy products
- Fructans: Found in many foods, including wheat, rye, barley, garlic, onions, dried fruit and legumes
- Galactans: Found in large amounts in legumes and some soy foods
- Polyols: Sugar alcohols found in some fruits and vegetables and often used as sweeteners
What role do they play in digestion?
During digestion, simple sugars (glucose and galactose) are absorbed into the bloodstream in the first few segments of the small intestine. Disaccharides (two simple sugars attached together) and other more complex sugars must be converted into simple sugars by digestive enzymes before they can be absorbed.
This digestive process is extremely efficient, so there is usually very little sugar left after the food has passed through the small intestine.
However, when sugars are poorly or incompletely digested during this process, they end up in the colon where they are subjected to the actions of the abundant bacteria found there. It is the intestinal flora that is responsible for the fermentation of sugars, and this phenomenon produces a lot of gas.
In people who are sensitive or suffer from IBS, this gas can cause bloating, abdominal pain and even diarrhea.
How to set up a low FODMAP diet
Kathryn Adel explains that a low FODMAP diet is usually recommended after a diagnosis of irritable bowel syndrome. Medical expertise is required to rule out more serious conditions such as celiac disease, Crohn’s disease or cancer.
The low FODMAP diet begins by eliminating FODMAD-rich foods, a process that lasts two to six weeks. “In less than 14 days, we can determine whether the diet is working,” says the dietitian. “The diet will be discontinued if no improvement is seen after two weeks.”
The second phase involves reintroducing specific foods to see which food families cause digestive disorders and at what threshold the symptoms appear. This testing phase allows us to isolate each FODMAPs family and identify those that are poorly digested.
Then, in the third phase, the patient can go back to eating almost as before, avoiding only the problematic foods.
“Usually, not all FODMAPs cause digestive problems. Identifying the most problematic ones and eliminating them are enough to improve the condition of patients,” says the specialist.
Risks and benefits
The dietitian believes that with professional care, the risks are almost non-existent. “Some people may find the reintroduction process long and difficult, others will experience some symptoms again, but in general, the relief obtained is very motivating.”
There are, however, a few dangers to following this diet without medical advice. “There is a risk of negatively affecting one’s intestinal flora or developing nutritional deficiencies if the diet is continued for too long. Some people are also going to have trouble performing the reintroduction tests themselves.”
Therefore, it is recommended to have a follow-up by a medical professional to maximize the chances of success of a low FODMAP diet. A website such as SOSCuisine.com is also an excellent source of help and information. Among other things, it can provide personalized menus for those following such a diet as well as support from specialized dietitian or self-service by an intelligent assistant to make reintroduction tests easier.
Foods to favour and avoid
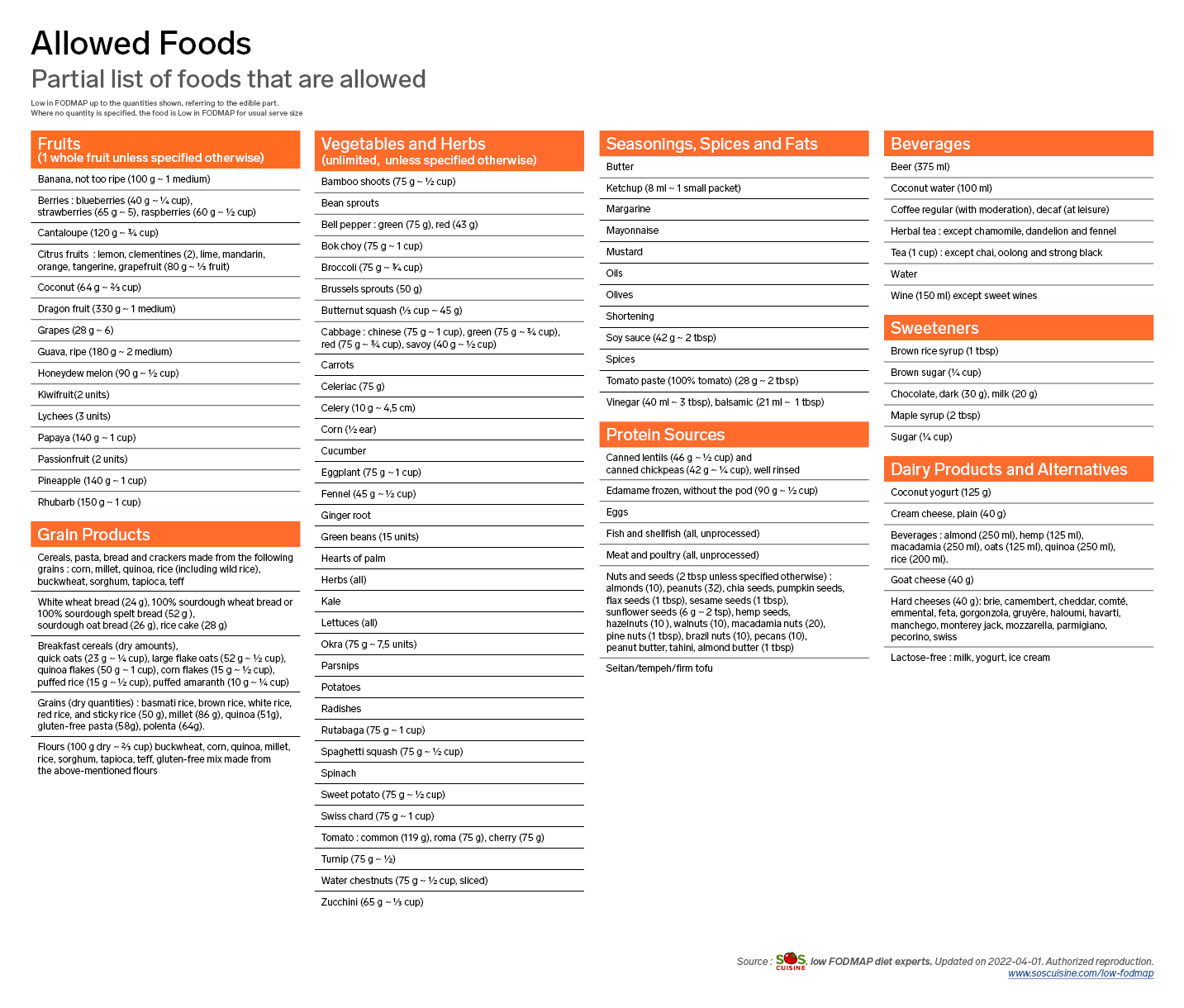
Some foods are particularly high in FODMAPs and should be avoided during the first two phases of the FODMAP diet.

Other foods, however, are low in FODMAPs and can be safely consumed in the amounts indicated during the first two phases of the FODMAP diet.
Effectiveness of the low FODMAP diet
Low FODMAP diet is often recommended to reduce the symptoms associated with many intestinal disorders, including IBS. According to Kathryn Adel, studies show an improvement in symptoms in about 75% of cases.1
There are also many treatments available to reduce the symptoms associated with IBS (e.g., psychosocial therapy, medications, etc.). A combination of treatments is most often the best way to find out which ones are most appropriate.[2] [3]
For professional support, we’re here for you.
We provide services that can help your doctor diagnose irritable bowel disorders and related health problems and determine the appropriate treatment.
- Fecal occult blood test
- Fecal calprotectin for chronic inflammatory bowel diseases detection
- Lactose tolerance test
- Celiac disease test
Do you have a medical prescription for any of these tests? Book an appointment online or contact Biron Health Group’s customer service at 1 833 590-2712.
Sources3
- H.M. Staudacher, K. Whelan (2017). “The low FODMAP diet: recent advances in understanding its mechanisms and efficacy in IBS,” GUT, 66:1517-1527, https://gut.bmj.com/content/66/8/1517.
- J. L’Écuyer. L’alimentation faible en FODMAP pour le syndrome de l’intestin irritable. https://hopitalmontfort.com/sites/default/files/PDF/alimentationfodmap_j.lecuyer.pdf (consulted March 10, 2022).
- A. Wald (2020). “Treatment of irritable bowel syndrome in adults,” UpToDate, https://www.uptodate.com/contents/treatment-of-irritable-bowel-syndrome-in-adults.










