Health A to Z — 10 minutes
Unequal menopausal symptoms and controversy surrounding treatments

Known for causing hot flashes and mood swings, menopause is a phenomenon whose repercussions on health and sexuality can be much more serious and complex than we think. For a long time, science has proposed two hormone-based treatments, but there is still a lively debate between supporters of traditional substitution on one side and those who favour bioidentical substitution on the other.
Causes and main symptoms of menopause
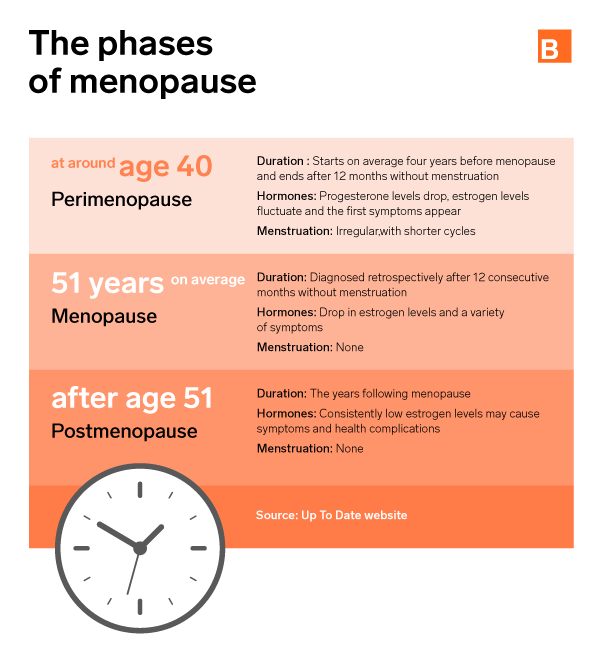
Menopause occurs in every woman’s life and is one of the noticeable effects of aging. Just like andropause in men, menopause happens when hormone production in the body decreases. Declining levels of estrogen and progesterone ultimately bring about the end of fertility (usually between the ages of 45 and 56).
Symptoms of menopause vary widely among women. Some may suffer a lot of distress during this period, while others may only experience minimal symptoms.
The most common symptoms include:
- Weight gain
- Hot flashes
- Insomnia
- Night sweats
- Vaginal dryness
- Joint pain
- Fatigue
- Short-term memory problems
- Intestinal problems
- Insufficient tear secretion
- Itchy skin
- Mood swings
- Urinary tract infections
These symptoms generally disappear or subside after menopause, between the ages of 50 and 60.[1]
How to diagnose menopause
In most women, the frequency of menstruation in the past 12 months as well as the symptoms history (hot flashes, etc.) is generally enough to diagnose menopause.
Depending on age (women under 45) or specific conditions (women taking birth control pills or undergoing a hysterectomy, etc.), laboratory tests can help determine whether the symptoms experienced are due to menopause or to a condition causing abnormalities in the menstrual cycle (beginning of pregnancy, overactive thyroid gland, high prolactin levels, etc.), or causing hot flashes (overactive thyroid gland, carcinoid syndrome, catecholamine-secreting tumours, etc.).
A natural phenomenon that sometimes involves complications
While menopause is not considered a “disease,” the drop in estrogen levels does increase the risk of developing health problems, such as:
- 2-6 fold increase in cardiovascular risk
- Bladder problems and possible incontinence while exercising, laughing or sneezing in 10-30% of postmenopausal women
- Sexual impairment due to reduced confidence, reduced desire or vaginal dryness[2]
The case of osteoporosis
Osteoporosis is a disorder characterized by the loss of bone mass and the breakdown of bone tissue. It is one of the natural consequences of aging and makes bones more fragile, thereby increasing the risk of fracture when impacted.
However, osteoporosis can affect any age group and sometimes develops as a result of certain cancers or their treatment. Menopause is also an aggravating factor for women due to the drop in estrogen levels. According to a report by the Public Health Agency of Canada, this disease affected more than two million people in Canada in 2016, 80% of whom were women. As a result, it is important for them to make sure their bones are in good condition during this time and afterwards.[3]
Treatments and debates around bioidentical hormones
Estrogen and progesterone supplementation has been used for decades to stabilize their decline during menopause. In recent years, some people have argued that there are two classes of hormones.
- The first involves administering traditional hormones to increase their level in the body.
- The second is called bio-identical or natural meaning that these hormones are of plant origin (soybeans). This name sometimes leads to a slight confusion and gives the false impression that they are naturally created hormones. They are in fact manipulated and chemically modified at some stage of their production. They are said to be identical, because the level of hormones would be identical to the one naturally generated by the body.
A documentary extolling the benefits of natural hormones
Loto-Méno, a documentary by Véronique Cloutier released in the summer of 2021, has reignited the debate on bioidentical hormones. In this miniseries the host discusses the challenges of perimenopause, the lack of information available on the subject and the benefits of bioidentical hormone therapy to treat the symptoms. She criticizes the fact that this more expensive treatment is not currently reimbursed by the RAMQ, whereas traditional hormones are.
Dr. Sylvie Godin, interviewed in the documentary, explains that these hormones would be preferable for women at risk of blood clots and over age 60. The hormones would also be more effective in treating certain symptoms (insomnia, mood swings, even anxiety and depression).[4]
Lingering questions in the field of research
In 2002, a major study by the Women’s Health Initiative (WHI) showed that hormones in combination with estrogen and medroxyprogesterone acetate increased certain risk of disease compared to a placebo treatment.
- Coronary heart disease: +29%
- Breast cancer: +26%
- Stroke: +41%
- Pulmonary embolism: +113%
Although the number of incidents in absolute terms was relatively low (less than 10 cases per 10,000 women treated in each category), the impact of this study on the medical community led to a considerable reduction in prescribing and administering this treatment at the time. The resulting therapeutic void opened the door to alternative treatments and bioidentical hormones in particular.
However, the numerous studies carried out so far have not shown any real differences in “performance” between the so-called traditional and bioidentical treatments. Comparison studies using placebos have even yielded substantially identical results in terms of reducing menopausal symptoms (mood swings, hot flashes, etc.). The Food and Drug Administration (FDA) in the United States and the Institut national d’excellence en santé et en services sociaux (INESSS) in Quebec consider that bioidentical treatment is neither safer nor more efficacious than traditional hormone replacement, and that this treatment does not justify the additional costs of bioidentical hormones.
The only certainty at this time is that consensus on the issue is far from established, and therefore science is continuing its research to improve hormone replacement treatments.[5]
How do we live with menopause
Menopause is a time of challenges and sometimes real suffering, and the treatments available are not always unanimously accepted, while some are even potentially dangerous. In addition, some symptoms can be caused by pathologies that are totally unrelated to menopause. Consequently, we must recognize that doubts persist, and questions remain.
However, we must not forget that each case is unique and therefore deserves a personalized approach to relieve or at least live better with the symptoms. The medical profession is increasingly aware, informed and equipped to deal with this issue. A medical opinion can therefore be a good starting point to evaluate the options available to you based on your condition.
Regardless of what happens, menopause remains a natural phenomenon and an unavoidable part of a woman’s life, an event that inevitably leads to changes in habits and daily life.
For professional support, we are here.
We offer services that can help your doctor determine if the symptoms you are experiencing are due to menopause or another condition and decide on the appropriate treatment. The most common tests are:
- FSH : FSH is associated with the menstrual cycle and ovum development in women and sperm production in men.
- Estradiol : This hormone is involved in regulating the menstrual cycle and helps maintain pregnancy. Estradiol is important in both men and women for bone growth and metabolism.
- TSH : TSH is a hormone produced in the pituitary gland that stimulates the production of hormones in the thyroid gland.
- Thyroid profile : A thyroid profile can detect most abnormalities affecting the thyroid gland or the secretion of TSH by the pituitary gland.
Do you have a medical prescription for one of these tests? Please book an appointment online or call customer service for Biron Health Group at 1-833-590-2712.
Sources6
- Canadian Women’s Health Network (s. d.). “Menopause.” https://cwhn.ca/en/faq/menopause
- Québec Blue Cross. (December 1, 2015). “Understanding menopause: Signs, symptoms and health concerns related to menopause.” https://qc.bluecross.ca/health-insurance/health-tips/620-understanding-menopause-signs-symptoms-and-health-concerns-related-to-menopause
- Government of Canada. (November 27, 2020). “Osteoporosis and related fractures in Canada: Report from the Canadian Chronic Disease Surveillance System 2020.” https://www.canada.ca/en/public-health/services/publications/diseases-conditions/osteoporosis-related-fractures-2020.html
- V. Cloutier (July 7, 2021). Documentary: “Loto-Méno.” https://ici.tou.tv/loto-meno
- L’actualité (June 30, 2021). “Tout sur les hormones bio-identiques.” https://lactualite.com/sante-et-science/tout-sur-les-hormones-bio-identiques/#quoi
- Journal of Obstetrics and Gynecology Canada. (May 28, 2016). “A Word About Bioidenticals.” https://www.jogc.com/article/S1701-2163(16)39221-0/fulltext








